CMS finalized a rule last month that will significantly expand access to telehealth services for patients in Medicare Advantage plans. Implementing provisions of the Bipartisan Budget Act of 2018 (BiBA), the new rule will allow patients to (finally) receive healthcare services from the comfort of their homes. According to CMS Administrator Seema Verma, “With these new telehealth benefits, Medicare Advantage enrollees will be able to access the latest technology and have greater access to telehealth.”
Medicare has long been an enigma for the telehealth community. With limited coverage options, arcane and complex rules, and the threat of massive fines and penalties for missteps, telehealth providers have understandably avoided involvement in Medicare. Most significantly, telehealth was not covered unless two nearly-impossible-to-meet criteria were met: that a patient be located in an “originating site” (which generally means a healthcare facility) and that the patient be in a county outside a Metropolitan Statistical Area or in a rural Health Professional Shortage Area (commonly referred to as a HPSA) in a rural census tract. As this map shows, these criteria substantially narrow the eligibility of patients to receive telehealth services and require them to go to a healthcare facility (where they are presumably already receiving healthcare services) to receive telehealth services. In fact, the OMB’s delineation of urban vs. rural counties results in only about 15% of the total US population being eligible for Medicare-covered telehealth services.
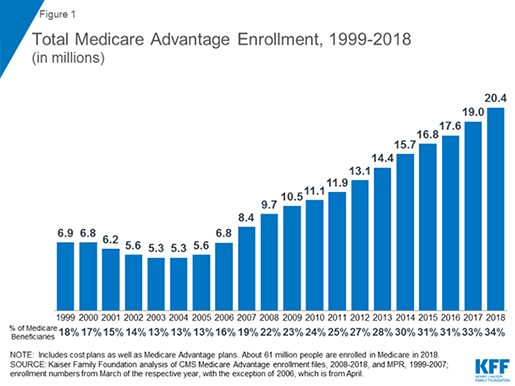
Although these barriers remain for Original Medicare, the BiBA removed these obstacles for Medicare Advantage plans starting in Plan Year 2020. Now, whether a patient is urban or rural, in their home or at their doctor’s office, they can receive telehealth services as a primary covered benefit under their Medicare Advantage plan. CMS notes that, “With these new telehealth and [non-health related] supplemental benefits, Medicare Advantage plans will have the flexibility to provide a historic set of offerings to beneficiaries.” This is really important. As the Kaiser Family Foundation explains, the percentage of Medicare beneficiaries in Medicare Advantage plans has risen precipitously since 2004, with over 34% now enrolled in a Medicare Private Health Plan.
This is great news for telehealth providers, as it opens up a substantial new patient population that historically purchases a lot of services and is becoming more comfortable with receiving services remotely. At the same time, it means that telehealth providers will need to adopt new strategies for remaining compliant. Many telehealth providers have grown accustomed to the Wild West of self pay and private insurance, where many of the laws related to their arrangements (i.e., Stark and the Anti-Kickback Statute) or billing practices (correct coding, mandatory claims submission) don’t apply (or at least aren’t enforced as vigorously). Although telehealth providers have become more compliance-oriented as they expand partnerships with Medicaid programs, Medicare is different. Medicare Advantage plans will “flow down” many compliance and auditing provisions that are required by CMS to contracted healthcare providers and telehealth providers will not receive a special exemption from this just because services are provided remotely. Instead, telehealth providers interested in working more closely with Medicare Advantage plans and their members will need to turn their regulatory compliance up to “11” to ensure they are effective partners with plans and good stewards of Medicare Trust Fund dollars.
Interested in more telehealth updates? Check out our May-rathon webinar on Advancements in Telehealth Law on May 22.